Navigating the Shadows: Unveiling Complex Post-Traumatic Stress Disorder (CPTSD)
- Jena Beck
- Aug 31, 2023
- 4 min read
Updated: Sep 19, 2023
Welcome back, lovelies. Last week, we dove deep into the shadows of Post-Traumatic Stress Disorder (PTSD). This time around, we're embarking on a journey to navigate an even more intricate maze – Complex Post-Traumatic Stress Disorder (C-PTSD). This variant of mental health challenges arises from prolonged, repetitive trauma within the realm of personal, intimate relationships.
CPTSD: Unveiling the Layers of Complexity
Complex Post-Traumatic Stress Disorder (CPTSD) unveils itself as a result of relentless exposure to repeated and prolonged trauma, casting its shadow on up to 7.3% of the population. Adverse Childhood Events (ACEs) and the Subtle Darkness of Intimate Partner Psychological Abuse
In the realm of trauma, shadows stretch across the spectrum of time, bridging past and present. Adverse Childhood Events (ACEs), like faint echoes from our formative years, often become the cornerstone of the intricate maze that is Complex Post-Traumatic Stress Disorder (CPTSD).
Understanding ACEs: Childhood Echoes
Before we delve into the subtler nuances of CPTSD within intimate relationships, it's crucial to grasp the significance of Adverse Childhood Events (ACEs). These events, ranging from emotional neglect to physical abuse and more, cast a long shadow that impacts our emotional landscape as we journey into adulthood. Approximately 1 in 6 adults experiences 4 or more types of ACEs. Early trauma exposure significantly increases the risk for many psychiatric disorders in adulthood, including complex post-traumatic stress disorder (C-PTSD). If you're interested in knowing your ACEs score, here's a link.
Intimate Partner Psychological Abuse: The Unseen Tyrant
While physical abuse often takes center stage in discussions of intimate partner violence, it's the insidious nature of psychological abuse that truly infiltrates the cracks of one's being. Starting small, like the gradual heating of water in a pot, abusers employ various tactics, from verbal insults eroding self-esteem to leveraging children and economic manipulation to establish dominance and control. Unlike physical wounds, the scars from psychological abuse may not be visible, but they cut deep.
The Intersection of ACEs and Intimate Partner Psychological Abuse
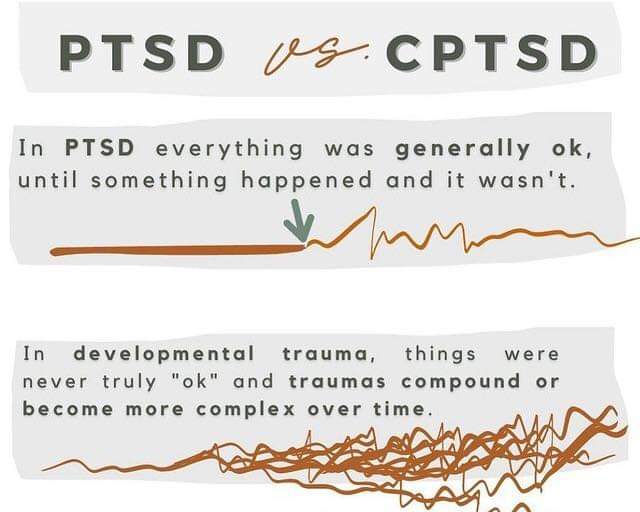
Historically, PTSD research spotlighted physical violence and life-threatening scenarios, inadvertently leaving the complex territory of CPTSD largely uncharted. But when ACEs cast their shadow, intertwining with intimate partner psychological abuse, the picture becomes multifaceted. CPTSD and PTSD may share similarities, but they are distinct entities. Born from the womb of trauma, they trigger flashbacks, nightmares, insomnia, and fear even in seemingly safe spaces. Yet, CPTSD weaves its own narrative, reprogramming the brain, body, and identity.
In upcoming discussions, we'll explore how ACEs disrupt regular brain development, creating a breeding ground for CPTSD's emergence. We'll shine a light on the intricate dance between childhood echoes and the shadows of intimate relationships, offering insight into the unique characteristics that set CPTSD apart. C-PTSD's Impact on the Brain: Unraveling the Ties That Bind
A hallmark of C-PTSD is the chronic sense of helplessness bred by prolonged trauma. This persistent feeling of entrapment isn't limited by gender and often plagues victims of intimate partner abuse who are trapped by financial or emotional dependencies. In future posts, we'll explore how childhood trauma intertwines with C-PTSD's emergence, disrupting typical brain development and catalyzing enduring changes in cognition, emotions, and social functioning.
Just like PTSD, ongoing emotional assaults from psychological abuse can shrink the hippocampus (key for memory and learning) and inflate the amygdala (the primal hub for emotions like fear, guilt, and shame). Moreover, C-PTSD's psychological abuse is linked to thinning the prefrontal cortex and temporal lobe – areas vital for self-awareness and emotional regulation. Over time, this abuse can degrade the hippocampus, fueling confusion, cognitive dissonance, and abuse-related memory lapses. The neurological architecture alterations and chemical imbalances from prolonged stress due to psychological abuse can contribute to heightened anxiety and depression. Here is a link to
Dwelling in a Realm of Fear: The Power of Psychological Abuse
Living in constant fear and anxiety, a reality for victims of psychological abuse, amplifies the amygdala's role. This 'lizard brain' governs essential functions like breathing, heart rate, and emotions, while also housing fear-based memories. These memories, influenced by stress hormones, become etched deeply in the mind. As a result, even minor triggers like scents, images, or words connected to the trauma can trigger cascading flashbacks. A Parting Thought: Shadows Can Fade
The scars of psychological abuse are etched deep within our minds. These echoes can persist for a long time, often requiring substantial effort to heal. In forthcoming posts, I'll dissect the red flags of psychological abuse, arming you with knowledge to spot them early. However, despair not. Our brains possess an incredible power – neuroplasticity.
Neuroplasticity, or brain plasticity, is the nervous system's ability to adapt in response to internal or external stimuli. Essentially, with proper therapy and support, our brains can process trauma, releasing what no longer serves us and embracing new coping mechanisms. Emotional nourishment is crucial during recovery from emotional abuse. Meditation, cognitive restructuring, and above all, self-love and compassion, play pivotal roles along the path to healing.
Until next time,
Jena
Mental Health Advocate and Herbalist
Disclaimer: This blog post is for informational purposes only and should not replace professional medical or psychological advice.
Sources: Redican, E., Marylene Cloitre, Hyland, P., McBride, O., Thanos Karatzias, Murphy, J., & Shevlin, M. (2022). The latent structure of ICD-11 posttraumatic stress disorder (PTSD) and complex PTSD in a general population sample from USA: A factor mixture modelling approach. Journal of Anxiety Disorders, 85, 102497–102497. https://doi.org/10.1016/j.janxdis.2021.102497
Reed, G. M., First, M. B., Joël Billieux, Marylene Cloitre, Peer Briken, Achab, S., Brewin, C. R., King, D. L., Kraus, S. W., & Bryant, R. A. (2022). Emerging experience with selected new categories in theICD‐11: complexPTSD, prolonged grief disorder, gaming disorder, and compulsive sexual behaviour disorder. World Psychiatry, 21(2), 189–213. https://doi.org/10.1002/wps.20960




Comments